According to the World Health Organization (WHO), every day almost 30,000 people suffer burn injuries that require medical treatment, i.e., 11 million a year worldwide.
The Institut de Recherche Biomédicale des Armées, CTIBiotech, the École Polytechnique and the Institut Pasteur are embarking on an unprecedented and highly innovative partnership to tackle this global health problem. Together, they hope to resolve a complex issue affecting serious burn victims: the superinfection of their wounds with Staphylococcus aureus, which often goes hand in hand with antibiotic resistance.
The Institut de Recherche Biomédicale des Armées specializes in monitoring and treating both military and civilian burn victims. As for the Ecole Polytechnique, it has developed the world’s first non-invasive, painless, and non-thermal cold plasma technology, which consists in exciting gas with electrical energy to create nitrogen and reactive oxygen species with healing, reparative and bactericidal properties. The Institut Pasteur is a clear expert in bacterial research, including the bacteria that infect serious burn injuries. Lastly, CTIBiotech is responsible for another world first: CTISkin™, an immunized human skin model produced using 3D bioprinting.
“Bioprinted skin models can be used to test different doses of cold plasma treatment, which produces more predictive human data before the clinical phase,” explains Dr. Nico Forraz, who founded CTIBiotech with Professor Colin McGuckin.
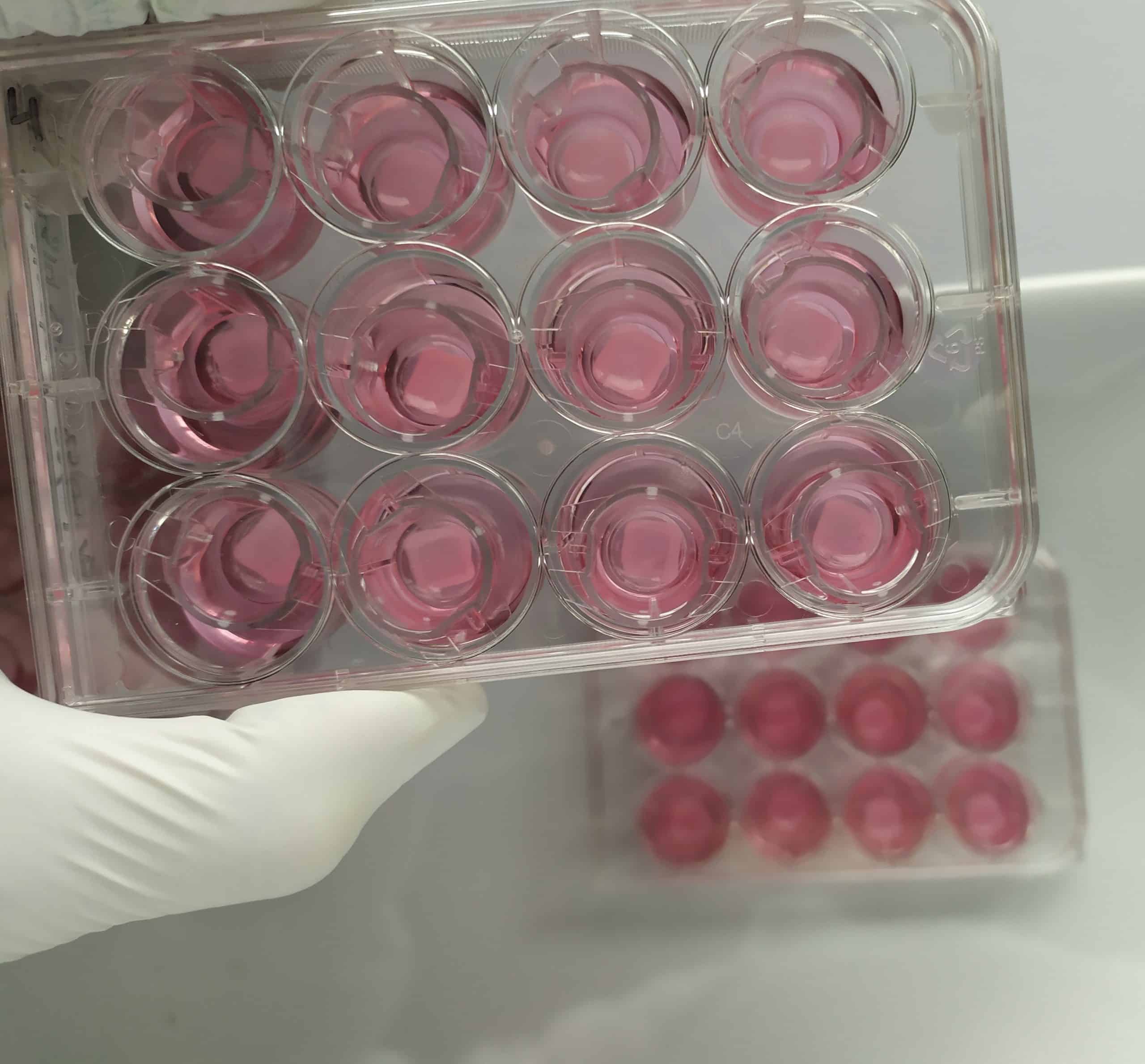
Since 2009, the Lyon-based company has focused on the 3D assembly of human cells to create predictive models for use in medical, pharmaceutical, or cosmetic research. Tissue from patients undergoing surgery – some of them cancer patients – is harvested for scientific research, with their consent. All of the skin cells are separated and sorted. Using laboratory cultures, tens of billions of skin cells are obtained from a one-centimeter square sample containing for example a million of each cell type. CTIBiotech then uses 3D bioprinting to produce complete skin models, with the possibility of adding other cell types, including immune cells, to the new skin segment. “This 3D printing technology increases the number of therapeutic approaches that can be tested for burn victims, for example,” explains Dr. Nico Forraz. Artificial lesions superinfected with an antibiotic-resistant bacterium are created on bioprinted skin models and treated using cold plasma technology.
This program will run for three years. The consortium hopes to enter clinical trials by the end of 2023.