Takayasu’s arteritis is an inflammatory disease of the blood vessels located in the aorta and its cervical and visceral branches and on the upper limbs. This rare disease affects 1,000 patients under the age of 50 in France, at a ratio of eight women for every man. It predominantly affects women and has been dubbed “pulseless disease,” because as it impacts subclavian arteries, it prevents any pulse being detected at the wrist. It is complicated by arterial stenoses and sometimes aneurysms.
Patients are generally monitored for 30 to 35 years, until they reach menopause, at which point the disease very often disappears. They are treated generally with anti-inflammatory drugs and antibody-based biotherapies that target inflammation molecules. But this gives rise to a number of problems. “The difficulty is in assessing inflammation of abnormally thickened arteries,” said Professor Tristan Mirault, Professor of Vascular Medicine at the Paris Cité University and Team Coordinator at the leading center for rare vascular diseases of the Georges-Pompidou European Hospital. “Female patients require a scan or MRI every three to six months. But these tools emit radiation, are expensive and not widely available.”
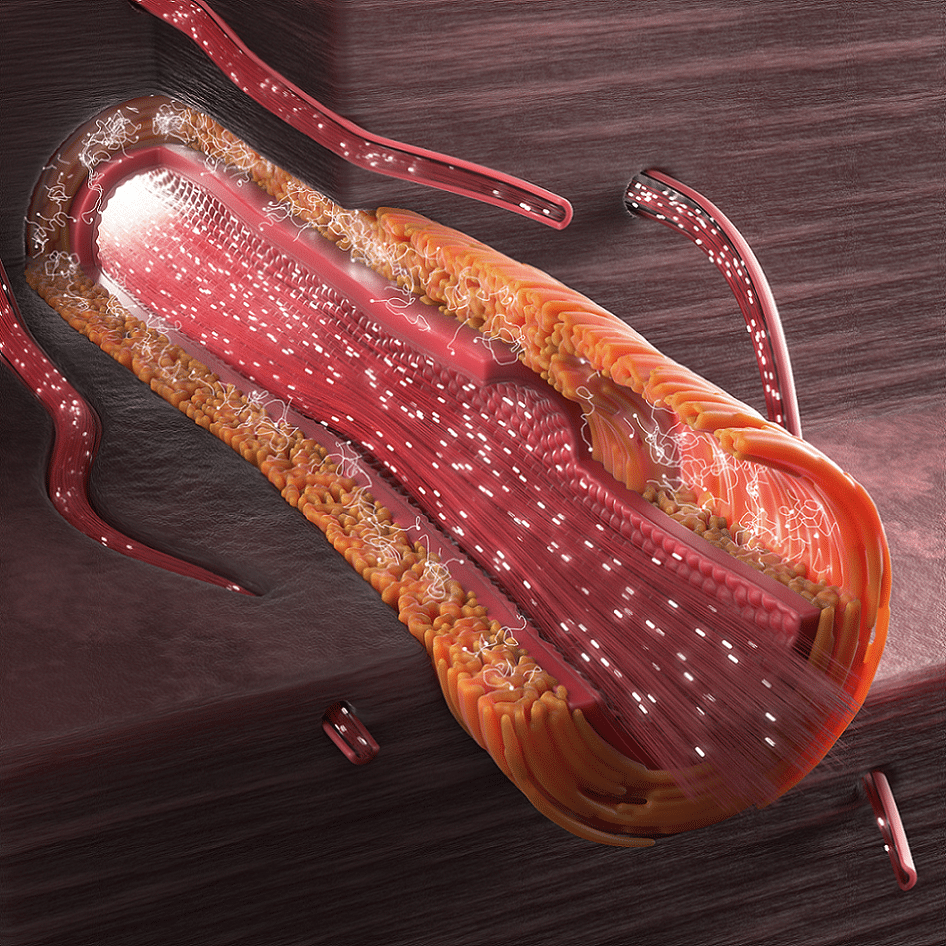
Scans are currently little used for this indication. However, ultrasound localization microscopy (ULM), based on ultrafast ultrasound imaging of circulating microbubbles, can image micron-sized microvascular blood flows in vivo down to the micron scale. The research team has thus sought to show that ULM can provide imaging markers to assess Takayasu’s arteritis activity. The team therefore relied on an innovation developed in the Physics for Medicinelaboratory at ESPCI Paris (Graduate School of Industrial Physics and Chemistry in Paris), led by physicists Mickael Tanter and Mathieu Pernot. They have developed a super-high-resolution ultrasound technology that goes beyond what can be seen with the naked eye.
“If this new ultrasound localization microscopy process (ULM) becomes easily accessible, we will be able to carry out scans to assess arterial wall inflammation using microbubbles. It is non-irradiating, low cost and very easy to access, as France has a huge number of scanning devices,” Professor Tristan Mirault, Team Coordinator at the leading center for rare vascular diseases of Georges-Pompidou European Hospital, Inserm and Paris Cité University.
This technique gives an idea of the vascularization of arteries and of their inflammation. The process has been applied on 16 male or female patients suffering from Takayasu’s arteritis. An initial traditional assessment was carried out to determine if the disease was in the active phase or not; then scans were used via the injection of microbubbles and the super-resolution technique. “We know that air reflects ultrasound very well, so we inject a liquid with microbubbles into the artery.”
SonoVue, an ultrasound contrast agent, contains tiny bubbles filled with sulfur hexafluoride gas. “We can then follow the progress of these bubbles in the artery wall and plot their route,” Professor Mirault added. Using the super-resolution technique, “we have observed the passage of the bubbles in the carotid artery walls, and have quantified, tracked and measured them.This was the first time this had been done!” the study coordinator reported.
The number of circulating microbubbles detected per second in the wall was 10 in quiescent cases versus 121 in active cases, with a mean velocity of 40.5 mm/s in active cases.
After the article was published in the March issue of the journal eBioMedicine, a number of manufacturers showed an interest in this new technique. Its field of investigation is indeed very wide as it can also be applied to tumor ultrasounds (kidneys, brain, thyroid, breasts, prostate, cutaneous tumors, etc.).
The results of another study, ULTRAVASC, are expected to be published by the end of the year. The same technology was used, but this time for atherosclerotic plaques in the carotid arteries. These can lead to stenoses, which may be operated upon to prevent stroke or to avoid recurrence. Plaque vascularization values will be compared with those found in histology. Fifty patients took part in the study. This plaque vascularization could serve as a marker of vulnerability for it and predict stroke-like complications.
Link to the study : https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(23)00067-1/fulltext